A groundbreaking diagnostic test is helping doctors unravel medical mysteries by analyzing DNA and RNA to detect a wide range of pathogens, including viruses, bacteria, fungi, and parasites. This advanced genomic test, developed by researchers at the University of California, San Francisco, is offering new hope in diagnosing cases where traditional tests fail to provide answers. The findings of two recent studies, published on Tuesday, highlight the potential of this technology in solving complex medical puzzles.
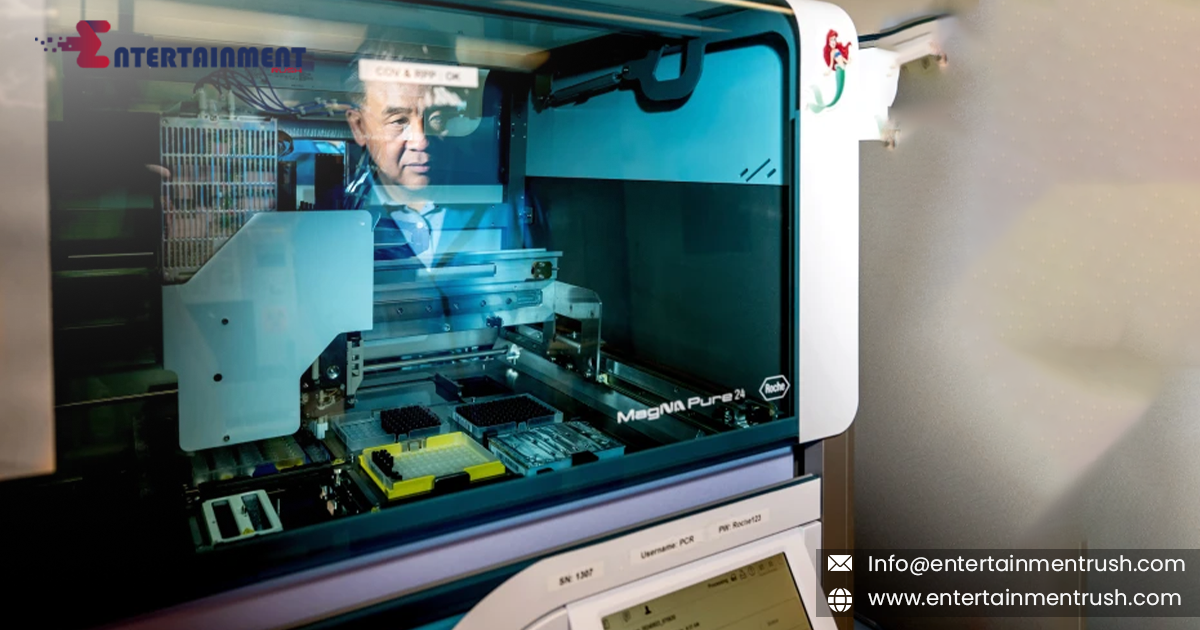
Unlike conventional diagnostic tests, which typically target specific substances like proteins, hormones, or genetic markers, this genomic test works by extracting all the DNA and RNA from a blood, tissue, or fluid sample. It then sequences the genetic material and compares it to a vast database of known pathogens to identify potential matches. While this test isn’t intended to replace common diagnostic tests for illnesses like COVID-19 or strep throat—due to its slower processing time and higher cost—it holds promise in more complicated cases, particularly when a patient exhibits severe symptoms, but initial tests return negative results.
The test has already proven effective in diagnosing neurological infections such as meningitis and encephalitis. According to one of the studies published in Nature Medicine, the test accurately diagnosed 86% of neurological infections in over 4,800 spinal fluid samples collected over seven years at UCSF. In 2021 and 2022, the test identified yellow fever as the cause of encephalitis in transplant recipients, tracing it back to their organ donors. The test also helped pinpoint the cause of a meningitis outbreak among patients who had undergone surgery in Mexico, identifying the fungus Fusarium solani.
In addition to identifying known pathogens, the second study published in Nature Communications suggests that the test could also detect novel viruses, including those that may have pandemic potential. Researchers conducted a simulation where they removed genetic sequences of known human viruses from the test’s database, yet the test was still able to identify related strains in animals, including the coronavirus that causes COVID-19.
While the test has received a “breakthrough device” designation from the FDA, which allows it to be used in clinical settings despite not yet being fully approved, it remains expensive, with each sample costing around $3,000. Currently, fewer than 10 labs use the test regularly, and it’s considered a “test of last resort” due to its high cost and labor-intensive process.
Despite its limitations, Dr. Charles Chiu, who led the development of the test, believes that its potential for diagnosing a range of conditions, such as pneumonia or sepsis, makes it a valuable tool in the future. However, Chiu acknowledges that more work is needed to make the test more accessible, including reducing the cost and improving turnaround times.
There are challenges ahead. According to Susan Butler-Wu, an associate professor at the University of Southern California, the technology may be too complex for community hospitals to adopt in the near future. Additionally, interpreting the results could be difficult for general practitioners, meaning that consultations with specialized laboratory directors would be necessary. Butler-Wu emphasizes that while the test can be a useful additional tool, it is not a one-size-fits-all solution and should be used alongside other diagnostic methods.
In summary, while this cutting-edge genomic test holds significant promise in identifying elusive pathogens and offering new insights into complicated medical conditions, its widespread use in hospitals is still a few steps away. Researchers are optimistic that, with time, this test could revolutionize the way we diagnose a variety of illnesses, but there are still hurdles to overcome before it becomes a standard part of clinical practice.